4) 화상의 진단(Diagnosis)
(1)화상의 범위(extent): 화상을 입은 부위를 전신 체표면적의 % (TBSA)로 표시한다. 이때 1도 화상을 제외한 2도 이상의 화상부위가 이에 해당된다.
a. 9의 법칙(rule of 9's) (Fig. 3) ; 빠르고 쉽게 범위를 계산할수 있어 응급실등에서 보편적으로 많이 사용하나 대략적인 계산으로 덜 정확하다. 유아와 어린아이에서는 연령별로 신체 각부위의 체표면적의 전신에 대한 %가 성인과는 다르다. 따라서 더 정확하게 하기 의해 하기에 기술한 챠트를 이용하는 것이 좋다.
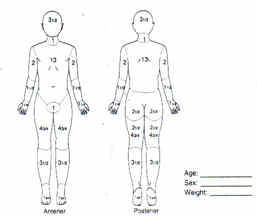
b.Lund and Browder chart; 화상범위를 연령별로 계산하며, 더 정확하며, 흔히 영구 의무기록 챠트에 사용된다.(Fig. 4)
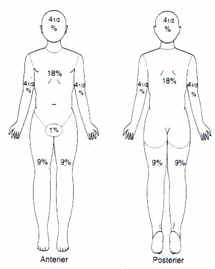
Fig.4. 9의 법칙(rule of 9's)
Fig.5. Lund and Browder chart
(2)화상의 깊이(Burn depth)
화상 초기에 깊이를 정확하게 판단하기 곤란한 경우가 많다. 따라서 깊이의 판단에
원인 물질이나 노출시간, 화상 원인등이 도움이 되기도 한다. 흔히 화염화상(flame burn)이 열탕화상(scalding burn) 보다 깊다. 또한 화학화상이나 전기화상의 경우 는 화상을 깊게 입지 않은 것 같이 보이지만 실제로는 심부 2도 화상 또는 3도인 경우가 흔하다.a) 화상 깊이의 분류
①1도 화상(1st degree burn,or superficial): 표피만 화상을 입는 경우로
흔히 일광 화상(sun burn)이 이에 해당되며, 홍반과 부종이 있다. 7 -10
치료에 치유된다.②2도 화상(2nd degree burn, or partial thickness); 표피는 물론이고 진피의 일부에 화상을 입은 경우이다. 이때 물집(blister, bullae)가 생기며, 이는 물집 하부의 진피의 일부가 손상된 것을 의미한다.
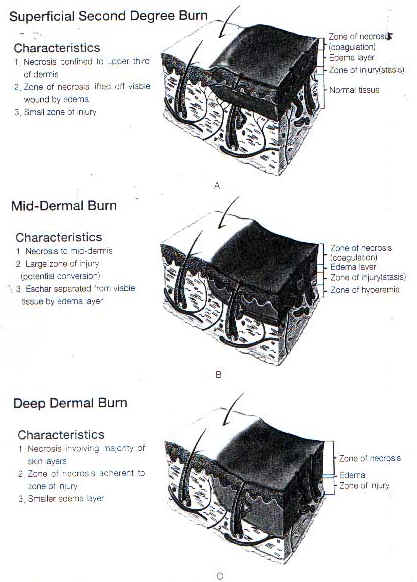
a.표재성 2도 화상(얕은 2도 화상, superficial second degree); 표피 전부와 진피의 상부 1/3 이내에 화상을 입은 경우로 진피의 유두층이 포함된다.가는 핀으로 찌르면 동퉁이 심하다. 흔히 10일 -2주에 치유된다.
*b.중간 2도화상(mid dermal burn)
표피와 진피의 1/3을 완전 포함하며 중간정도의 진피 손상이 있느경우로, 적당한 동통이 있으며 2-4 주의 치유기간이 요하며,환부의 conversion의 위험이 높다.
c.심부 2도 화상(깊은 2도 화상 deep dermal burn): 진피의 망상층 일부까지도 화상을 입는 경우로 대부분 진피의 2/3의 깊이가 손상된 경우이다. 자연 창상치유가 서서히 일어나며 3-8주 정도에 치유된다. 가피제거를 위해 수술적 시술이 요하기도 하며, 흉터가 심하게 남을수 있다. 심한 염증이 발생되면 흔히 2도 화상으로 전환된다.
③3도화상 (3rd degree burn, full-thickness);피부 전층의 화상으로 밀랍 같은 흰색,또는 혈전으로 인한 갈색등의 색조를 띄며, 마른 가죽 같이 건조하며, 동통이 없다.피부 전층의 소실로 상피화는 되지 않으며, 창상치유에 피부이식술이 필요하며, 적은 범위(2-3cm 직경)의 환부에서만 창상 구축에 의해 치유될수 있다.
④4도화상(4도 degree burn): 피부 전층은 물론 심부조직인,건, 근, 골 까지도 화상을 입은 경우이다.흔히 사지 절단술, 피판 전이술, 복합조직이식술등을 사용하여 재건하게 된다.
화상의 깊이의 구별에 중간 2도화상의 구별은 주로 화상센터 또는 화상 전문 치료기구에서 많이 시행하고 있으며, 또한 깊이의 판단이 어려운 경우의 2도 화상에서 Indeterminate thickness의 구별을 두기도 한다. 이는 실제적으로 중간 2도화상 및 심부 2도 화상이 혼재되어 있는 경우와, 심부 2도화상 및 3도 화상이 혼재되어 발생된 경우가 이에 해당되며 두 경우 모두 화상깊이의 전환(conversion)의 위험도가 높은 특징을 가지며, 이에 따라 치료의 유형이 달라지기도 한다.
Fig.6. 화상의 깊이. 2도 화상의 세분류 Fig.7. 2도화상(상), 3도화상(하)의 모습
Table 3. 화상의 깊이(Burn depth) 판단
|
Burn degree |
Cause |
Surface appearance |
Color |
Pain level |
|
First
|
Flash flame, ultaviolet |
Dry, no blisters, no or minimal edema |
Erythematous |
Painful
|
|
Second |
Contact with hot liquieds or solids, flash flame to clothing, direct flame, chemical, ultraviolet |
Moist blebs, blisters
|
Mottled white to pink, cherry red |
Very painful
|
|
Third
|
Contact with hot liquids or solids, flame, chemical, electrical
|
Dry with leathery eschar until debridement ; charred vessels visible under eschar |
Mixed white, waxy, pearly; dark,khaki, mahogany; charred |
Little or no pain; hair pulls out easily
|
|
Fourth ( involves underlying structure ) |
Prolonged contact with flame, electrical
|
Same as third degree, possibly with exposed bone, muscle, or tendon |
Same as third degree
|
Same as third degree |

3) 화상은 유아나 노인에서 더욱 심한 이환율(morbidity)과 사망률(mortality)을 보인다. 특히 환자의 나이가 3세 미만이거나 60세 이상에서 더욱 그러하다.
(4)위치: 안면부. 경부, 수족부, 회음부는 특별한 문제를 야기할 수 있고(e.g. 눈꺼풀 화상은 각막의 노출 위험이 있으며,회음부는 감염이 잘됨), 따라서 주의를 요하며 때로는 입원을 필요로 한다.
(5) 흡입화상의 유무: 밀폐공간, 코털의 그을음, 인후의 탄소가루, 쉰 목소리, 결막염.
(6)골절, 두부손상등의 동반손상의 유무
(7)동반되는 이환요인(co-morbid fatctors)로는 순환기, 호흡기, 신장, 대사성 질환; 발작성 질환, 알코올중독, 약물남용등이 있다.
(8)예후: 화상입은 면적, 연령,화상의 깊이나 흡입화상과 연관 지어 판단.
(9)윤상 화상(circumferential burn)이 있는 경우 응급으로 가피절개술 시행이 필요하다.
5) 응급처치
화상환자의 응급처치는 다른 외상환자의 처치와 마찬가지로 전신적으로 이루어 져야 한다.
우선적으로
1)환자 도착즉시 기도유지(maintenance of a patent airway)를 시행하여 효과적인 호흡(ventilation)을 할수 있도록한다. 흡입화상(inhalation injury) 또는 상기도 화상(upper air way burn)이 있을시엔 기도삽관(endotracheal intubation)을 시행한다. 환자가 응급실 도착즉시에 비교적 쉽게할 수 있는 기도삽관도 화상부종(burn edema)과 치료과정의 많은 양의 수액투여로 인하여 매우 어려워 질수 있어 이에 대한 대비를 하여야한다..
2) 전신적 혈액 순환(systemic circulation)이 정상적으로 유지되도록 한다.
3) 다른 외상 또는 손상이 동반될수 있다. 즉 두부손상(head injury), 기흉(pnemothorax) 등의 흉부 손상,척수 손상(spinal injuries), 장파열(ruptured viscus), hemoperitoneum, retroperitoneal hemorrhage등과 같은 복부 손상(intraabdominal injuries), 골반골 및 장골의 골절(pelvic & long bone fracture), 과도한 출혈 등에 대해 평가를 해야 된다. 환자는 흔히 다소 혈압이 높을수 있다. 그러나 초기에 설명하기 어려운 저혈압을 보이거나 전신적 혈액?감소(systemic hypovilemia) 증상이 있으면 어떠한 다른 손상이 발생되어 있는지의 가능성에 대해 유의해야 한다.
4) 병록과 신체검사(history & physical exam)
5) 중화상 환자의 전문적 화상환자치료시설(burn care facility)로 환자이송의 경우는 심각한 다른 손상에 대해 처치후 기도유지한후 신속히 한다.
6) 흡입화상의 응급처치;
흡입화상은 화상환자의 사망하는 주요한 원인중 하나이다. 흡입화상이 확인되면 사망율은 30-40% 증가된다. 흡입화상이 의심되면 조기에 기도삽관을 시행하는 것이 호흡부전(respiratory distress)의 방지에 도움이 된다. 이의 진단은 임상적으로 확실치 않은경우가 많으며, 혈액검사상 동맥혈 가스분석중 carboxyhemoglobin(CHgb)가 10% 이상의 소견이 있으면 진단 가능하다. 특히 집안의 화재에서 환자가 사망하는 가장 많은 원인이 일산화 탄소 중독증으로 알려져 있어 이에대한 대비가 필요하다. 흔히 일산화 탄소 중독이 의심되면 환자 후송시에 100% 산소 흡입이 도움을 줄수 있으며, 응급실에서 single chamber 혹은 double chamber등의 oxgen tank를 사용하여 치료할수 있다. 이때는 의사가 곁에서 밀접한 관찰아래 시행되어야 하며 항상 microembolism에 대한 평가를 시행하여야한다.
5) 입원의 적응증(Indication for admission)
화상환자의 이환률(morbidity) 적게 하기 위해서 화상센터 또는 화상환자치료실(burn unit)가 설비된 병원 또는 치료기관에서 무엇보다 경험이 풍부한 화상전문의의 지시아래 치료계획이 필요하며, 여기에는 성형외과의, 일반외과의, 응급의학과, 마취과, 소아과의, 정신과의, 물리치료사,화상간호사, 화상치료사, 사회사업가등으로 구성된 의료팀이 가동하여 치료에 적합한 여러 모니터 장치, 공기정화소독기, Air bed 혹은 Air fluidaized silicon bed(Clinitron) 침상을 갖춘 병실, 와류욕조등을 가진 창상 처치실, 소수술실등을 겸비한 시설에서 적절하게 환자를 치료를 하는 것이 좋다.
Table 5. 화상센터 및 전문적 화상치료 시설을 갖춘 병원으로의 입원 조건
--------------------------------------------------------------------------
Second and third degree burns >10% body surface area (BSA) in patients <10 or >50 years old.
Second and third degree burns >20%BSA in other groups.
Second and third degree burns with serious threat of functional or cosmetic impairment that involve face, hands, feet, genitalia, perineum, and major joints.
Third-degree burns <five% BSA in any age group.
Electrical burns, including lightening injury.
Chemical burns with serious threat of functional or cosmetic impairment.
Inhalation injury with burn injury.
Circumferential burns with burn injury.
Burn injury in patients with pre-existing medical disorders that could complicate management, prolong recovery, or affect mortality.
Any burn patient with concomitant trauma ( for example fractures ) in which the burn injury poses the greatest risk of morbiidity or mortality. However, if the trauma poses the greater immediate risk, the patient may be treated in a trauma center initially until stable, before being transferred to a burn center. Physician judgement will be necessary in such situations, and should be in concert with the regional medical control plan and triage protocols.
Hospitals without qualified personnel or equipment for the care of children should transfer burned children to a burn center with these capabilities.
--------------------------------------------------------------------------
6) 치료계획(Treatment plan)
환자가 의식이 있는 경우는 간단히 처치방법을 소개하고 다음 사항에 의해 중화상환자(major burn)의 입원처방(admission order)을 낼 수 있다.
(1).병록과 신체검사(history & physical exam); 수상 당시의 상황, 환자의 다른 질환의 기왕력, 현재의 상용하고 있는 약품, 과민반응 등의 알레르기 증상에 대해 조사하며, 이학적 검사는 완전 탈의한 상태에서 전신의 모든 부위에 대해 손상이 있는지를 검사한다.
(2).호흡곤란을 해소하기위해 가피 절개술(escharotomy) 혹은 기도 삽관
a) 윤상화상(circumferential burn)을 입은 경우, 특히 흉부의 원형의 가피는 호흡곤란을 가져오며 양측 전액와선(anterior axillary line)에 가피절개술을 시행하여 준다. 사지 및 수부에 발생된 원형의 가피는 이의 원위부에 혈류를 차단하여 구획증상(compartment syndrome) 또는 사지의 원위부 허혈과 괴사를 일으킨다.이를 검사하기 위해 수지 또는 족지에서 도플러(Doppler) 기구를 사용하여 맥박을 측정할수 있다. 또는 16G - 주사바늘을 사용하여 Prick test를 하여 선홍색의 모세혈관 의 출혈(bleeding) 이 되면 적당한 혈류순환이 있음을 알수 있으며, 출혈이 되지 않거나 서서히 되면 동맥혈부전(arterial insufficiency)가 있음을 알수 있다. 산소분압이 95mmHg 이하인 경우도 혈류의 장애를 의미하며, 즉시 가피절개술이 필요하다. 가피절개술은 전체 가피의 길이와 깊이에 걸쳐 시행하여 피하조직이 충분히 노출되어야하며, 구획(compartment) 부위에서는 근막절개술(fasciotomy)까지 시행한다.
b)가피절개술의 적응증으로는
a. 청색증(cyanosis) b. 느려진 모세혈관 재충전(impaired capillary refilling), c.점진적인 신경학적 변화(progressive neurologic change(paresthesis, deep tissue pain)) d. 촉지할수 있는 맥박의소실(loss of palpable pulse), 도플러 맥박의 소실(abscence of Doppler pulses), 구획압력(compartment pressure) 가 30mm Hg 이상인경우이다. 가피절개술후에는 원위부에서의 혈류순환을 확인해야하며, 충분한 가피절개술후에도 혈류순환이 되지 않으면 수액요법이 불충분한지를 확인하여야한다.
(3)화상 쇽(burn shock) 을 예방하거나 처치: 굵은 바늘로 IV line을 확보한다. (4)모니터 소생법(monitor resuscitation)을 위해 도뇨관을 삽입하여 시간당 뇨량을 잰다.
(5)20%이상의 화상일 경우 위장관(nasogatirc tube) 삽관; 장마비(ileus), 구토를 처치 한다.
(6)파상풍(tetanus) 예방:
(7)기초 검사(Baseline Laboratory studies:)
Hct., 뇨검사(UA),혈당검사( FBS), BUN, 흉부 엑스선(chest x-ray), 전해질(electrolytes), 심전도(EKG), cross-match, 동맥혈가스검사(arterial blood gases)시행, carboxyhemoglobin(흡입화상 의심시) 수치 측정 등
(8)화상창상의 세척및 치료를 한다.
7) 흡입화상(inhalation injury)
화상 사망률의 주요한 원인(20-80%)을
차지한다. 일반적으로 화상과 흡입화상이 동반되면
사망률은 2배가 된다.
(1)흡입화상의 3 종류:
a) Co2 흡입(inhalation):무색, 무취인 C02는
헤모글로빈에 산소보다 210배의 친화성
(affinity)을 가지고 있다.
b) 상기도 위장관에 직접 열화상(direct
thermal injury to upper aero-digestive tract);
이 때는 기도부종은 흔히 18-24시간에
최고에 다다르다 수상후 4-5일에
가 라앉게된다..
c) 연소 물질의 흡입에 의한 smoke burn; 흡입 화상의 가장 흔한 원인으로 우리의 주변 환경은 여러 물질로 구성되어 여기에 불이 붙어 발생된 다양한 유해 화학물질(noxious chemicals)에 의해 손상을 입는다. 알데하이드(aldehydes), 케톤(ketone), 유기산(organic acids)등이 이러한 물질에 해당되며 기도에 심각한 화학화상을 일으킨다. 심한 기관지수축(bronchoconstriction)등을 일으키며 Pco2 가 상승된다.점막의 섬모기능(mucosal ciliary function)이 급격히 저하되며 secretion의 clearence 기능히 저하된다. 흔히 하기도(lower respiratory tract)에 잘 발생되며 모세혈관 투과성(capillary permeability)의 변화, 폐포 세포(alveolar cell)의 괴사등으로
폐부종, 호흡부전 증후군(respiratory distress syndrome)에 빠지며 60-70%의 사망률을 보이게 된다. 수상후 72시간 경과후에 이차감염의 발생이 되면
환자 상태는 더 나빠지게 된다.
(2)진단;폐쇄된 공간에서의 화상병력, 그을리거나 탄 콧털, 안면 및 구개인두강의 화상, 탄소가루 섞인 가래등이 있게되며 재채기를 하게된다.
상기도 폐쇄의 증상인 인후두부의 손상으로 인해 목쉰소리(hoarsness),
협착음(stridor),천명(wheezing), 공기 공복(air hunger)등의 증상을 보이기도 한다.경우에 따라 상기한 증상이 심하지 않는 경우도 있으며, 모든 흡입화상의 의심이 되는 환자에서 CHgb을 측정하여 10% 이상이면 강력히 의심하여야하며, 만약 CHgb 수치가 50%이상이면 흔히 사망하게된다. 산소분압 자체는
높게 유지되더라도 실제 조직내의 산소 운반능력은 낮은 경우가 있어
이 데이터의 분석에는 조심이 필요하다.(3) 진단의 도구로는 응급으로 상기도 검사에 굴곡성 내시경적 기관경
( fiberoptic bronchoscopy)을 시행하며, 하기도 손상엔 Xenon lung scan,
페기능검사(pulmonary function test)가 비교적 진단에 도움이 된다.
수상 당시의 흉부 X-선 사진은 진단에 별다른 도움이 안되며,
흔히 수상후 1 - 2 일 경과후는 흉부 x-선으로도 평가할수 있다.(4)치료: 기도유지, 기관삽입, 기관절개술(tracheostomy)후 100% 산소 투여, endotracheal suction, bonchoscopy등을 사용한 빈번한 폐 세척(pulmonary toilet), ventilator를 사용한 postive end respiratory pressure(PEEP)등으로 호흡을 유지한다. 또한 수상후 3-10일간 항생제(antibiotics)등을 투여하여
이차 감염을 치료한다.